Heart Transplant
A heart transplant, while it may be a moment of sadness from one side with the Donor, it is a time of overwhelming joy for the Recipient. A heart transplant, as it says, is taking a diseased heart and replacing it with the donor heart. Timing is essential for the donor heart, as many advancements have been made to prolong the time a heart can live outside of the body, sometimes either on ice which has been the norm for years prior to today's "Heart in a Box" invention.
Most heart transplants are done on patients who have end stage heart failure, a condition in which your heart is severely damaged or weakened, and on people who have failed other treatment options. Criteria is based hospital to hospital and there are instances in which exceptions have been made if patients do not necessarily meet the requirements. Some of the requirements and or contraindications include but are not limited to:
- The severity of the heart disease, as to what degree of heart failure does the candidate have.
- Other medical options that could be available other than a transplant.
- Other diseases, co morbidities in which the patient might also have (Systemic Disease, Cancer, Smoker, Substance Abuse, HIV)
- Age (65-70) depends on the facility as well as on the patient profile.
- Height and Weight (Either morbidly obese or cachexia are contraindications)
- The ability for the candidate to stick to the treatment before and after transplantation. A strong psychosocial support system is vital as well.
- Severe Pulmonary Hypertension/Dysfunction
- Recent CVA
- Psychiatric Instability
Being listed for a heart transplant comes after the immense amount of testing is done. Depending on the case and the patient profile they are placed in 1 of 3 catagories:
- 1A: Currently in the hospital on inotropes, currently on a VAD with a malfunction/infection.
- 1B: Patient on inotropes either at home or hospital and/or on VAD support
- 2: Patient living at home able to carry on ADL's
- 7: Patient listed but bot accruing time
For a patient to become a donor, aside from being medically "brain dead" they as well need to meet certain requirements as well as having contraindications.
- Age: 13-50 (40 for male and 45 for female require cardiac cath)
- Hep B to Hep B donor-recipient
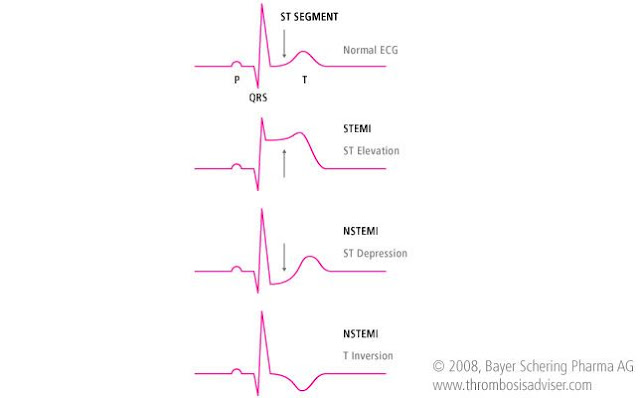
- Risk Factors (drug use, Hx of Arrhythmia's, Hx of MI, HLD, HTN)
- Central Venous Pressure <15
- Ischemic time less than 4hrs
Tissue Compatibility from Donor to Recipient need to be completed. Blood Typing as they need to match as well as determining their PRA(Panel Reactive Antibody) percentage which basically determines the chance and/or amount of a reaction the recipient might have upon transplantation. The donor heart is denervated so it is unable to respond to direct sympathetic and parasympathetic activation. medications like Atropine are ineffective.
Surgery begins with a sternotomy (Opening the sternum/chest). The diseased heart is removed.
Depending on patient and/or surgeon and contrary to common belief, a portion of the old diseased heart may be left inside the patient and the new donor heart will be cut to fit the portion of the recipients old heart. Another method would be a Total Heart transplant, where the entirety of the old heart is removed and replaced with the new one. Below shows examples of the BiCaval and BiAtrial Approach, both of which have their pro and cons.
Post transplant, many changes need to be introduced into the patients life. Medications that need to be taken on a strict schedule, dosing of those medications, monitoring for rejection is a major post transplant complication, decreasing the introduction of opportunistic infections, cardiac rehab, diet changes.
3 types of rejection can occur:
- Acute Cellular Rejection: when the T cells in the body attack the cells of the heart.
- Oral/IV Corticosteroids and Thymoglobulin
- Acute Antibody Rejection: The body creates antibodies towards the hearts cells, interpreting them as "foreign invaders".
- Oral/IV Corticosteroids
- Plasmapheresis which filters out all of the bodies antibodies, the good and bad. IVIG are given to replenish them.
- Chronic Rejection: develops over time with the presence of Cardiac Allograph Vasculopathy (Accelerated form of CAD which cause luminal narrowing of the Coronary Arteries)
If any of your patients present with:
- Fever/Flu Like Symptoms
- HTN
- Edema
- Change in HR
- SOB
PASS IT ON TO THE ATTENDING PHYSICIAN/NP/PA
Upon arriving to the unit, the patient will have Central Lines, Chest Tubes and other drains, Foley catheters etc.
Along with the corticosteroids, patients have to take anti rejection medications for the rest of their lives. As nurses we need to teach them the side effects and when to call their LIP when something arises.
Tacrolimus and Cellcept are 2 of the most common medications given to transplant patients.
- Tacrolimus: Labs are drawn to check the levels of Tacrolimus to determine the dosing. Over time the dosage will decrease as the body becomes "accustomed" to the foreign organ. Side Effects include Renal Impairment, HTN, HLD, Hyperglycemia and Tremors. Limit foods high in potassium as well as salt substitutes, Grapefruit Juice due to it decreasing the potency of the drug as well as other nephrotoxic medications.
- Cellcept: Handle as if a chemotherapeutic agent. Reactions include Nausea,Vomiting and Diarrhea.
- Nystatin
- Bactrim
- Valganciclovir
Biopsy's, Echo's are done to determine the level of rejection post transplant. There will always be some sort of rejection to determine the level of decrease in the patients immune system. NO rejection at all could mean the immune system is being shut down completely and the patient is at a greater risk for opportunistic infections. To high of a rejection and patient risks the chance of losing the organ and a lesser chance of survival.
AVOID!
- NSAIDs
- Grapefruit Juice and Pomegranate
- Herbal products
- Others who are sick and wear an N95 face mask when out in a busy public place.
- Tanning beds (higher risk for the development of cancer)
- Live Vaccines
Patient typically return to their normal lifestyle after completing some sort of Cardiac Rehabilitation.
Any questions?! Message me on my Instagram @thenursenel or Email nelrn22@gmail.com






Comments
Post a Comment